October 8, 2025
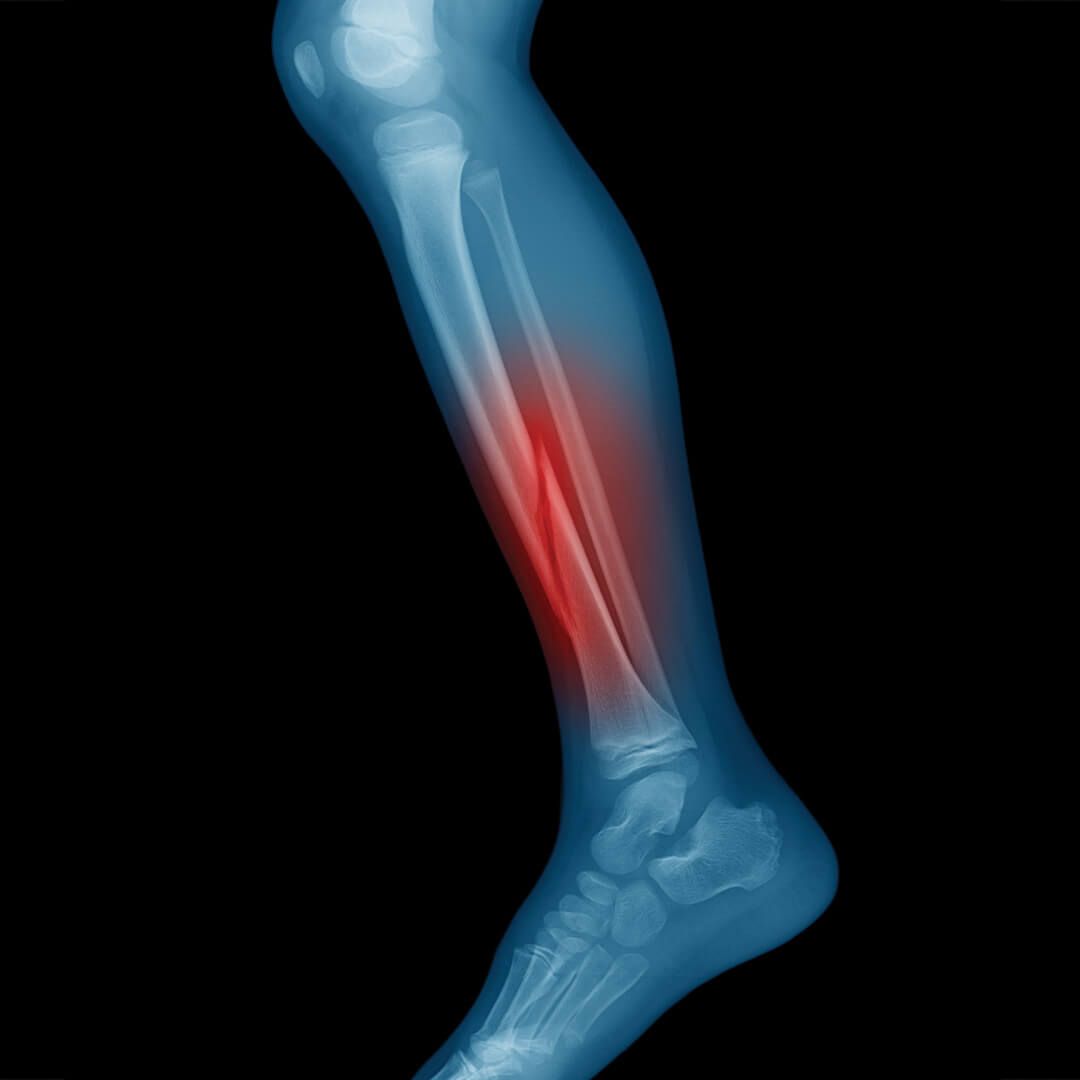
Lipoedema and lymphoedema are conditions that can significantly affect daily comfort, mobility, and self-confidence. Both involve abnormal fluid accumulation, but for different reasons: Lipoedema is a chronic condition characterised by abnormal fat and fluid deposition, usually in the legs and sometimes arms, causing heaviness, tenderness, and disproportionate limb size. Lymphoedema is caused by impaired lymphatic flow, leading to fluid retention, swelling, and tissue changes, often after surgery, trauma, or as a primary condition. While medical management is essential, complementary therapies can help reduce discomfort, improve mobility, and support lymphatic function. One such effective therapy is Brazilian Lymphatic Drainage (BLD). Unlike traditional lymphatic drainage, BLD is firm, continuous, and dynamic, specifically designed to move stagnant fluid, reduce tissue congestion, and improve circulation. It also provides sculpting and contouring effects, helping limbs feel lighter and more comfortable. How Brazilian Lymphatic Drainage works The lymphatic system is the body’s natural drainage network, responsible for removing fluid, toxins, and metabolic waste from tissues. In lipoedema and lymphoedema, fluid can accumulate due to tissue changes or impaired lymphatic flow, causing heaviness, swelling, and discomfort. BLD works by: • Using firm, wave-like, continuous movements to mobilise fluid from congested tissues • Directing fluid toward lymph nodes where it can be efficiently cleared • Reducing tissue congestion while improving circulation to affected areas • Supporting detoxification and tissue health • Promoting sculpting and contouring effects, especially in the legs, arms, and abdomen Unlike light lymphatic massages, BLD applies dynamic pressure that encourages deep fluid movement and tissue mobilisation, making it especially effective for chronic conditions like lipoedema and lymphoedema. Benefits of BLD for lipoedema and lymphoedema Helps reduce swelling and heaviness BLD’s firm, continuous strokes help move fluid from congested areas toward the lymph nodes, reducing swelling in the legs, arms, and glutes. Many clients notice a measurable reduction in heaviness and limb circumference after a few sessions, making mobility easier and daily tasks more comfortable. Helps to improve circulation and tissue function Enhanced lymphatic and blood flow ensures that tissues receive oxygen and nutrients while waste products are cleared. For individuals with lipoedema or lymphoedema, this can reduce discomfort, tenderness, and inflammation while supporting tissue health. Helps support lymphatic and fluid clearance BLD helps reactivate lymphatic flow in areas affected by impaired drainage. This is especially important for lymphoedema patients, whose lymphatic systems may struggle to clear excess fluid effectively. Regular sessions help maintain consistent fluid movement and reduce the risk of fluid build-up. Provides sculpting and contouring effects BLD’s firm, flowing strokes target affected areas, helping limbs feel lighter and more contoured. For lipoedema, where fat deposition can be uneven, BLD assists in mobilising fluid and easing tissue tension, which can improve overall limb shape and comfort. Helps reduce discomfort and tenderness Both lipoedema and lymphoedema can cause pain, tenderness, and a heavy sensation. BLD helps relieve pressure in congested tissues, reduces tightness, and promotes a sense of lightness in the limbs, making daily movement easier. Helps enhance overall wellbeing Beyond physical relief, BLD promotes a sense of comfort and relaxation. While it is firm and dynamic, clients often feel energised, lighter, and more in control of their bodies after a session. This can improve confidence and quality of life, particularly for individuals managing chronic swelling. What a Brazilian Lymphatic Drainage session involves A typical BLD session for lipoedema or lymphoedema lasts 45–60 minutes and includes: Firm, continuous, wave-like movements on the affected limbs, glutes, abdomen, and sometimes the arms Focus on mobilising fluid toward key lymph nodes, including inguinal, axillary, and cervical nodes Dynamic pressure designed to move stagnant fluid effectively, not just superficially Particular attention to areas prone to congestion, such as thighs, calves, or forearms Clients may notice lightness, reduced swelling, and improved mobility After a session, many people experience increased urination as the body clears excess fluid, a lighter sensation in the limbs, and reduced tension or tenderness. Frequency and consistency For best results, regular BLD sessions are recommended: Weekly or biweekly sessions can help maintain lymphatic flow and reduce recurrent swelling Consistent treatment supports tissue health, fluid balance, and mobility Over time, regular BLD can improve the long-term appearance, feel, and function of affected limbs Consistency is especially important for lipoedema and lymphoedema, as these are chronic conditions where fluid retention can return without ongoing support. Complementary strategies BLD works best alongside supportive lifestyle measures: Hydration: Adequate water intake supports lymphatic clearance Movement: Gentle exercises like walking, swimming, or cycling improve circulation and reduce congestion Compression garments: For lymphoedema, these may be recommended to support fluid control after sessions Balanced nutrition: Anti-inflammatory and nutrient-rich foods support tissue health and minimise fluid retention Stress management: Techniques such as meditation, deep breathing, or yoga complement BLD’s benefits Who may benefit BLD can help: Individuals with lipoedema or lymphoedema seeking relief from swelling and heaviness People who experience tenderness or discomfort in congested areas Those wanting dynamic, effective therapy to support lymphatic function and body contouring Anyone looking for improved mobility, comfort, and confidence while managing chronic swelling BLD is complementary and should be used alongside medical management for lipoedema or lymphoedema. Always consult a healthcare provider for personalised care. Final thoughts... Living with lipoedema or lymphoedema can affect comfort, mobility, and confidence. Brazilian Lymphatic Drainage offers a firm, dynamic, and highly effective way to mobilise fluid, reduce swelling, ease tenderness, and support lymphatic function. Regular BLD sessions, combined with hydration, movement, and appropriate medical support, provide a holistic approach to managing these chronic conditions. Beyond physical relief, clients often experience increased energy, improved mobility, and a renewed sense of control over their bodies. By targeting the abdomen, pelvis, glutes, and limbs, Brazilian Lymphatic Drainage addresses fluid congestion at its source, promoting long-term comfort, balance, and wellbeing.